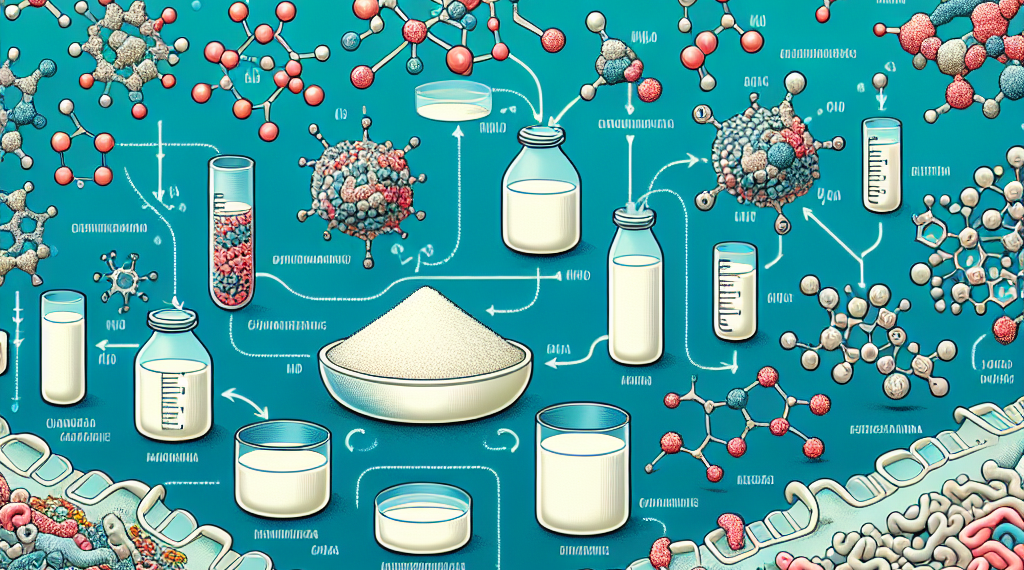
When we think about the benefits of human breast milk, we often focus on its nourishment for infants. However, a component of breast milk known as human milk oligosaccharides (HMOs) is now gaining attention for its potential health benefits beyond infancy. HMOs are complex carbohydrates that, while not digestible by babies, play a critical role in developing their immune systems and shaping the gut microbiota. But what about their effects on older children and adults? A new study has delved into this question, exploring how HMOs influence the gut microbiome and the production of health-related metabolites.
The Power of HMOs in Gut Health
The research reveals that even at low doses, between 0.3 to 0.5 grams per day, HMOs can significantly boost the production of short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate in both children and adults. These SCFAs are more than just waste products; they are vital molecules that our gut bacteria produce. They serve various functions, including nourishing colon cells, regulating immune responses, and reducing inflammation. Butyrate, in particular, is a superstar for colon health, serving as the primary energy source for the cells lining the colon and possessing anti-inflammatory properties.
Specific HMOs and Their Unique Benefits
The study also highlights the distinct effects of different HMO structures. For instance, lacto-N-neotetraose (LNnT) was found to be especially effective in ramping up butyrate levels. Meanwhile, 6’Sialyllactose (6’SL), another HMO, had a more pronounced impact on propionate production. These findings are crucial because each SCFA has unique health implications, and understanding which HMOs boost their production can help tailor dietary interventions for specific health outcomes.
Beyond SCFAs: A Broader Impact on Health
HMOs don’t stop at increasing SCFA levels. The study found that they also enhance the production of metabolites related to immune function and the gut-brain axis, as well as vitamins. This is exciting because it suggests that HMOs could influence not just gut health but also neurological functions and mood-related symptoms through their impact on neurotransmitter-related metabolites.
Low Doses, Big Impact
Remarkably, the beneficial effects of HMOs were observed at relatively low doses. Just 0.5 grams per day was enough to stimulate the growth of Bifidobacteriaceae, a family of bacteria known for their positive role in gut health. This is significant because it suggests that even small amounts of HMOs in the diet could help maintain a healthy and diverse gut microbiome, which is linked to a lower risk of various diseases, including obesity, type 2 diabetes, and certain cancers.
The Role of Cutting-Edge Technology
The insights from this study were made possible by the use of Simulated Intestinal Fluid Reactor (SIFR®) technology. This innovative method allows researchers to mimic human gastrointestinal conditions in the lab, providing a closer look at how substances like HMOs interact with the gut microbiome.
Looking to the Future
The implications of this research are far-reaching. As we understand more about how HMOs affect gut health in people of all ages, we can begin to consider their inclusion in dietary supplements or functional foods. This could open up new avenues for preventing and managing various health conditions through diet, emphasizing the importance of maintaining a healthy gut microbiome for overall well-being.
In conclusion, the study’s findings underscore the potential of HMOs to positively influence gut health and beyond. As research continues to unfold, we may soon see new dietary strategies that harness the power of these remarkable breast milk components to improve health across the lifespan.